The Oral Polio Vaccine (OPV) has been a cornerstone in the global effort to eradicate polio, a highly infectious and debilitating disease that has plagued humanity for centuries. As we move forward in 2025, it is essential to review the current state of OPV, its history, benefits, and challenges, as well as the ongoing efforts to improve its efficacy and accessibility.
History of OPV
The development of OPV dates back to the 1950s, when Dr. Albert Sabin created a live, attenuated vaccine that could be administered orally. This innovation revolutionized polio vaccination, as it was easier to administer, less painful, and more cost-effective than the inactivated poliovirus vaccine (IPV) developed by Dr. Jonas Salk. The introduction of OPV led to a significant decline in polio cases worldwide, and by the 1980s, the number of reported cases had decreased by over 90%.
How OPV Works
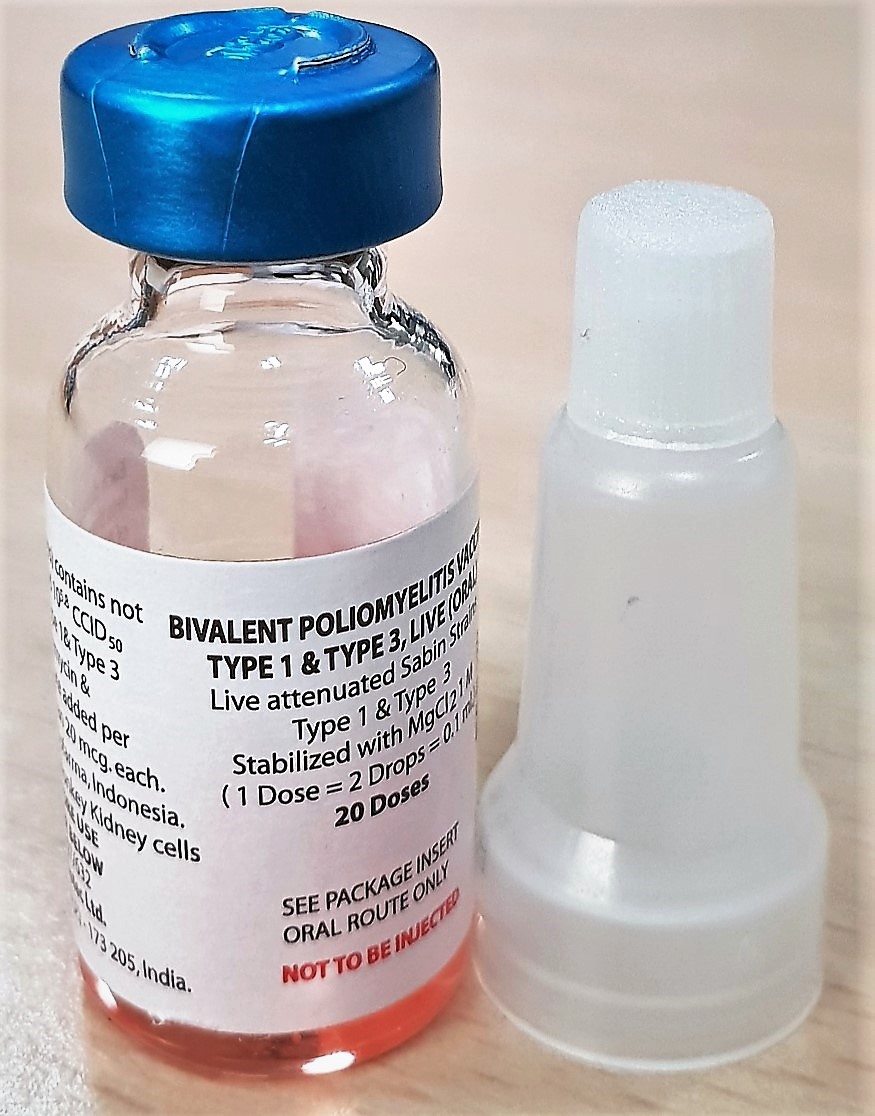
OPV contains a weakened form of the poliovirus, which, when ingested, replicates in the gut and triggers an immune response. This response produces antibodies that protect against future infections, providing immunity to the individual and helping to prevent the spread of the virus. OPV is typically administered in multiple doses, with the first dose given to infants at 2 months of age, followed by booster shots at 4, 6, and 18 months.
Benefits of OPV
The benefits of OPV are numerous:
- High efficacy: OPV has been shown to be highly effective in preventing polio, with a single dose providing immunity in over 90% of recipients.
- Convenience: The oral administration of OPV makes it easier to deliver, especially in areas with limited access to healthcare facilities.
- Cost-effectiveness: OPV is significantly cheaper than IPV, making it a more viable option for low-income countries.
- Community protection: OPV not only protects the individual but also helps to prevent the spread of the virus in the community, reducing the risk of outbreaks.
Challenges and Limitations
While OPV has been instrumental in reducing polio cases, it also has some challenges and limitations:
- Vaccine-associated polio: In rare cases, OPV can cause vaccine-associated paralytic poliomyelitis (VAPP), a condition that can lead to paralysis.
- Vaccine-derived poliovirus: The weakened virus in OPV can, in rare instances, mutate and cause outbreaks of vaccine-derived poliovirus (VDPV).
- Immunodeficiency: Individuals with weakened immune systems may not respond effectively to OPV, leaving them vulnerable to infection.
- Cold chain requirements: OPV requires a strict cold chain to maintain its potency, which can be a challenge in areas with limited infrastructure.
Recent Developments and Improvements
To address the challenges associated with OPV, researchers and manufacturers have been working to improve its efficacy and safety. Some recent developments include:
- New vaccine formulations: Researchers are exploring new vaccine formulations that can provide better immunity and reduce the risk of VAPP and VDPV.
- Improved manufacturing processes: Advances in manufacturing have led to the development of more stable and potent OPV, reducing the need for frequent booster shots.
- Introduction of novel vaccine technologies: New vaccine technologies, such as inactivated poliovirus vaccine (IPV) and synthetic poliovirus vaccines, are being developed to provide alternative options for polio vaccination.
FAQ
Q: Is OPV still effective in preventing polio?
A: Yes, OPV remains a highly effective vaccine in preventing polio, with a single dose providing immunity in over 90% of recipients.
Q: What are the risks associated with OPV?
A: The risks associated with OPV include vaccine-associated polio, vaccine-derived poliovirus, and immunodeficiency.
Q: Can OPV be given to individuals with weakened immune systems?
A: No, OPV is not recommended for individuals with weakened immune systems, as they may not respond effectively to the vaccine.
Q: How is OPV administered?
A: OPV is typically administered orally, in multiple doses, starting from 2 months of age.
Q: What is the difference between OPV and IPV?
A: OPV contains a live, attenuated virus, while IPV contains an inactivated virus. OPV is easier to administer and more cost-effective, while IPV provides a stronger immune response and is recommended for individuals with weakened immune systems.
Conclusion
The Oral Polio Vaccine (OPV) has been a crucial tool in the global effort to eradicate polio. While it has its challenges and limitations, the benefits of OPV far outweigh the risks. As we move forward in 2025, it is essential to continue improving the efficacy and safety of OPV, as well as exploring new vaccine technologies and formulations. With ongoing research and development, we can work towards a future where polio is a disease of the past, and OPV plays a vital role in achieving that goal.
By addressing the challenges associated with OPV and continuing to improve its efficacy and accessibility, we can ensure that this life-saving vaccine remains a cornerstone of global health efforts for years to come. The progress made in polio vaccination is a testament to the power of collaborative efforts and innovative solutions, and we must continue to build on this momentum to achieve a polio-free world.
Closure
Thus, we hope this article has provided valuable insights into Oral Polio Vaccine (OPV): A Comprehensive Review. We thank you for taking the time to read this article. See you in our next article!