Understanding how individuals respond to immunizations or infections is critical for several reasons:
- Vaccine Effectiveness: Evaluating antibody levels after vaccination helps determine the potency of the vaccine and its ability to provide sustained protection.
- Personalized Medicine: Antibody titers can inform medical decisions by revealing an individual’s immune status and susceptibility to certain diseases. This allows for tailored interventions, such as booster shots or prophylactic treatments.
- Disease Surveillance: Monitoring antibody prevalence in populations provides valuable information about disease spread and potential outbreaks.
This article delves into the intricacies of antibody response monitoring, exploring its various techniques, clinical applications, and future directions.
Methods of Antibody Response Monitoring:
Several methods are employed to quantify and analyze antibody responses:
- Enzyme-Linked Immunosorbent Assay (ELISA): This widely used technique detects and measures the presence of specific antibodies in a patient’s blood serum. ELISA involves coating a plate with the target antigen, adding the patient’s serum, and then detecting antibody binding using an enzyme-linked secondary antibody.
- Neutralization assays: These assays directly measure the ability of antibodies to neutralize a pathogen.
- Immunofluorescence Assay (IFA): This method uses fluorescently labelled antibodies to visualize antigen-antibody binding on cells or tissues.
- Flow cytometry: This technique analyzes individual cells, allowing for the identification and quantification of antibody-expressing cells.
- Next-generation sequencing (NGS): This advanced method can be used to identify and quantify the diverse repertoire of antibodies produced by an individual.
Clinical Applications of Antibody Response Monitoring:
Antibody response monitoring finds numerous applications in clinical practice:
Vaccine Efficacy Evaluation:
Immunization programs rely on antibody titers to assess vaccine effectiveness. Measurable antibody levels indicate successful vaccination, providing protection against the specific pathogen.Boosting Strategies: Antibody levels naturally decline over time. Monitoring titers helps determine the need for booster shots to ensure sustained immunity.
Infection Diagnosis: Elevated antibody levels against a specific pathogen can confirm an active or past infection.
Immunodeficiency Assessment: Individuals with compromised immune systems may have difficulty mounting an adequate antibody response. Antibody levels can help diagnose and monitor immunodeficiency disorders.
Autoimmune Disease Management: Monitoring antibody levels involved in autoimmune diseases allows physicians to track disease activity and adjust treatments accordingly.
Transplant Monitoring: Antibody levels against donor organs can indicate rejection risk. Monitoring helps tailor immunosuppressive therapy and prevent organ failure.
Challenges and Future Directions:
Antibody response monitoring faces several challenges:
- Standardization: There is a need for standardized protocols for antibody testing to ensure accurate and comparable results across different laboratories and studies.
- Longitudinal Studies: Tracking antibody responses over time is crucial for understanding immune durability and informing vaccination strategies.
- Correlates of Protection: Identifying the precise antibody levels required for protective immunity against specific pathogens remains a complex research area.
Future advancements in antibody response monitoring include:
Development of point-of-care tests: Portable and rapid antibody tests could facilitate timely diagnosis and treatment decisions.
Personalized vaccination approaches: Tailoring vaccination schedules based on individual antibody profiles could optimize immune responses.
Therapeutic antibody development: Understanding antibody structure and function is critical for developing effective antibody-based therapies for various diseases.
FAQ:
Q: How long does it take to develop detectable antibody levels after vaccination or infection?
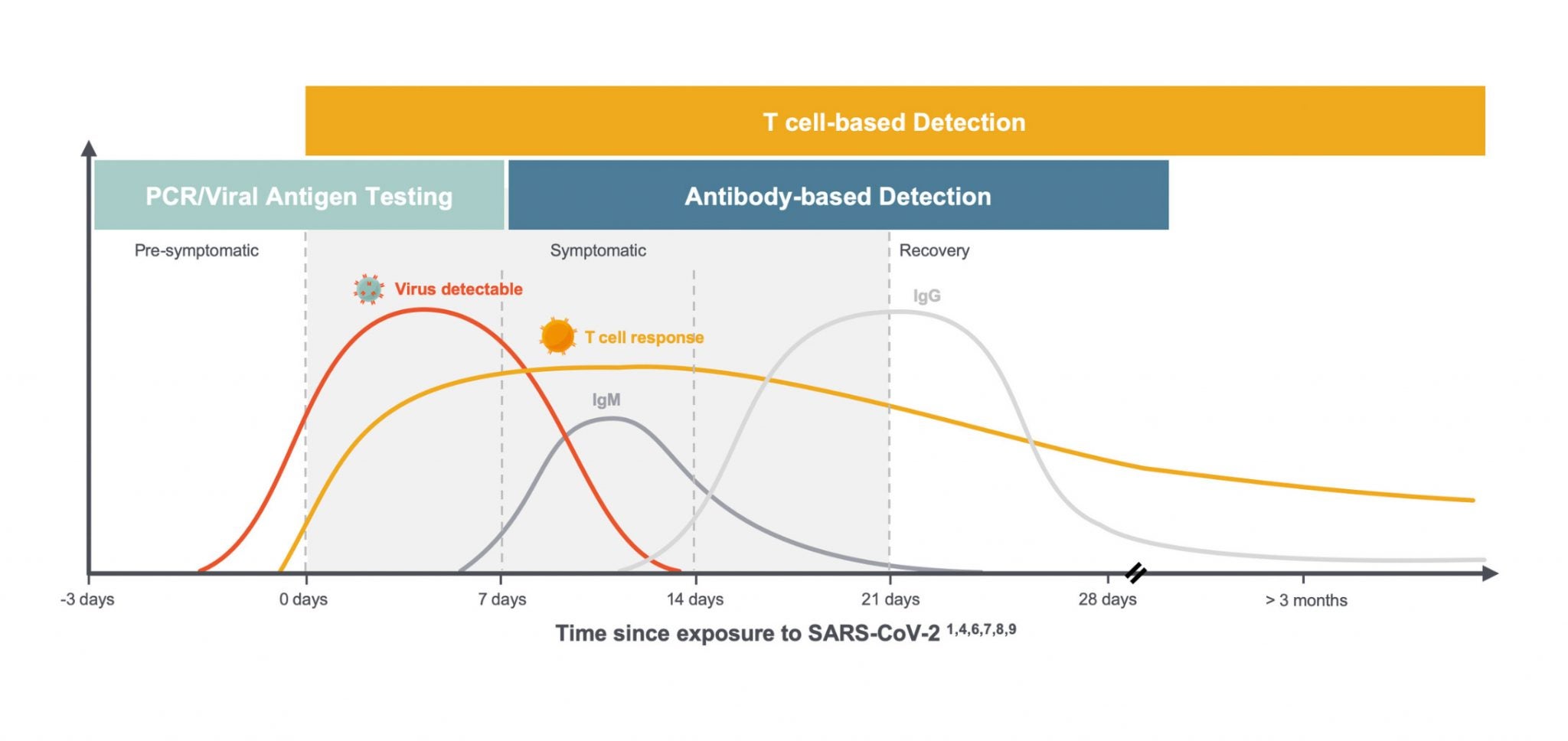
A: The time required for antibody levels to become detectable varies depending on the pathogen, individual immune response, and type of vaccine. Generally, it takes a few weeks for significant antibody titers to develop.
Q: How long do antibody levels remain protective?
A: Antibody-mediated immunity wanes over time. The duration of protection varies amongst individuals and pathogens. Booster vaccinations are often recommended to enhance and sustain immunity.
Q: Can antibody response monitoring predict disease severity?
A: In some cases, antibody levels can provide insights into disease severity. However, this is not always straightforward as other factors also play a role.
Q: Is antibody response monitoring a painful procedure?
A: Antibody testing typically involves a blood draw, which can be associated with mild discomfort.
Conclusion:
Antibody response monitoring is a powerful tool for advancing vaccine development, personalized medicine, and our understanding of the human immune system. By accurately measuring antibody levels, we can tailor immunization strategies, inform clinical decision-making, and ultimately improve disease prevention and treatment outcomes.
As research advances, we can anticipate even more innovative applications of antibody response monitoring, paving the way for a future of precision healthcare.
Closure
Thus, we hope this article has provided valuable insights into Antibody response monitoring. We appreciate your attention to our article. See you in our next article!